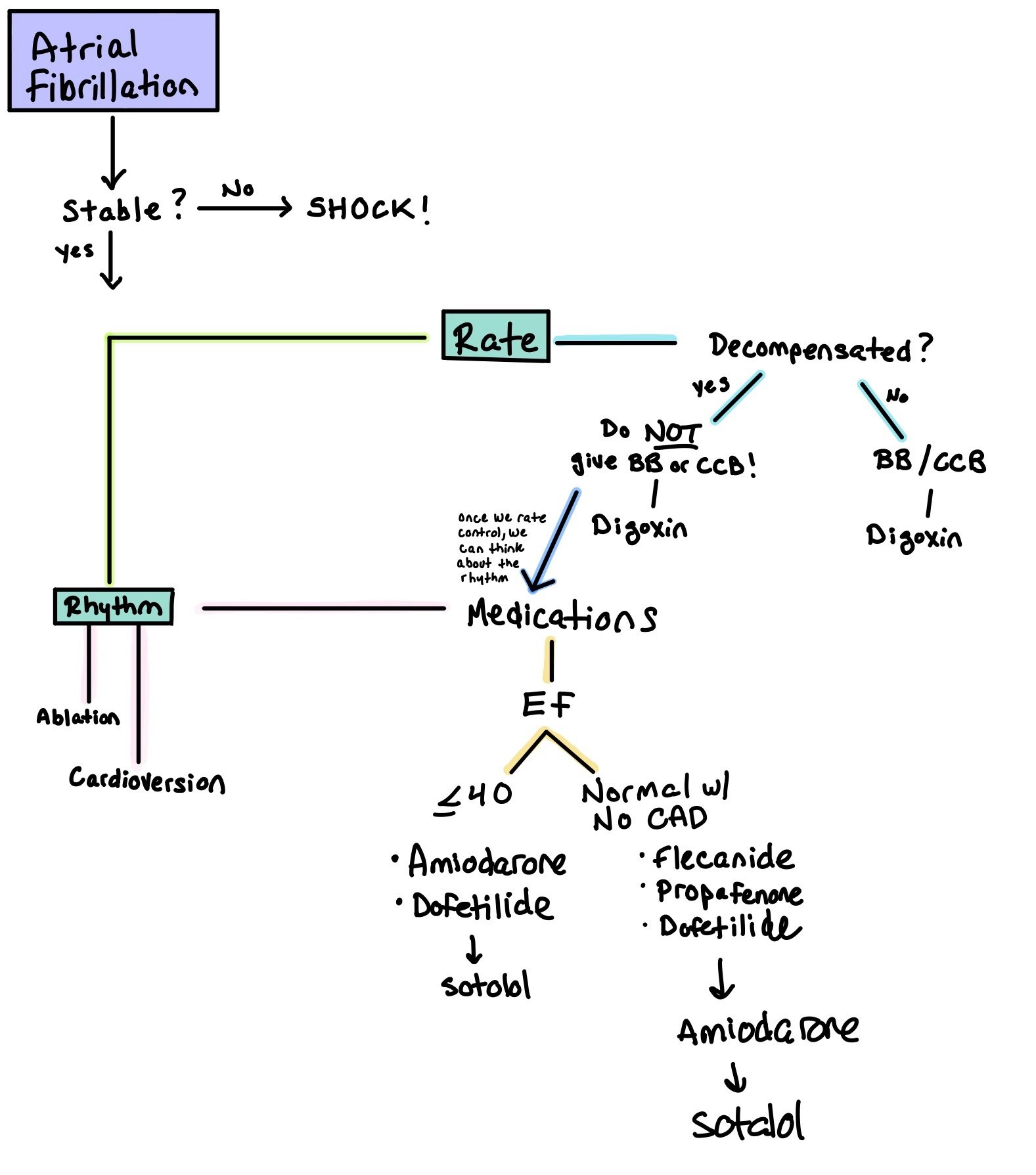
When patients are in AF, the first step is to determine whether or not the patient is stable. If the answer is no, SHOCK!
Remember, all patients who get shocked need to be on anticoagulation for at least 1 month as cardioversion causes atrial stunning.
The next step is to determine if the patient should have rate or rhythm control. Ultimately, rhythm control has been shown to be superior to rate control (EAST-AFNET 4). However, in the acute setting, rate control may be used.
Rate Control:
Is the patient decompensated?
If yes, do NOT give beta blockers or calcium channel blockers!! This will only decompensate them more. If you do, give SHORT ACTING (such as esmolol).
If no, try a beta blocker or calcium channel blocker.
Regardless, digoxin can be used when all other rate control fails.
Medications:
Class 1C: Blocks Na channels; decreases conduction velocity and impulse formation.
Note: These medications MUST be used with a beta blocker or non-dihydropyridine calcium channel blocker to prevent conversion of afib into 1:1 atrial flutter.
Flecainide:
Pro: Relatively safe for patients who have structurally normal hearts
Con: Cannot be used in patients with structurally abnormal hearts
Dosing: PO 50-200 mg Q12h
Considerations: For patients who have a very low burden of afib, flecainide can be taken as a PRN when patients feel they are in afib, aka as Pill in Pocket. Note: they should not take more than 1 dose in 24 hours. Dosing 200 mg (weight < 70 kg) or 300 mg (weight ≥ 70 kg) PRN for paroxysmal AF
Propafenone
Dosing: PO IR 150-300 mg Q8h, ER 225-425 mg Q12h
Considerations: Pill-in-pocket: IR 450 mg (weight < 70 kg) or 600 mg (weight ≥ 70 kg) PRN for paroxysmal AF (no more than 1 dose in 24h)
In the CAST investigation, class 1C antiarhythmics (flecanide and encainide) were associated with an increased mortality in patients with recent MI. Of note, most of these patients had EF <50%. In CASH, propafenone shown to have similar effects. As such, guidelines recommend that patients with previous MI or significant structural heart disease do NOT get prescribed 1C agents due to concerns for increased mortality and worsening heart failure.
Class II: Prolongs phase 4 of the action potential, causing increased conduction time and refractory periods. Also blocks sympathetic input to the SA and AV nodes
Beta blockers (metoprolol, carvedilol)
Pro: Come in PO and IV form. Works relatively quickly
Con: Will stay in the system and can cause bradycardia and hypotension. Can cause heart block. As these are negative chronotropic agents, they should be used with caution in patients with acute heart failure.
Dosing: Can give up to
Carvedilol up to 25mg BID
Metoprolol 200mg/day or 1mg/kg/day
Considerations:
Cardioselective: atenolol, bisoprolol, metoprolol, nadolol
Class III antiarrhythmics: blocks K channels, causing delayed repolarization; prolongs QTc interval
Amiodarone
Pro: Has both alpha and beta blocking properties and affects Na, K, and Ca channels. Very easy to use. Can be used in patients with structural heart disease. Comes in both oral and IV formulation. Very long half life so good in patients who miss doses
Cons: Many side effects, including thyroid, liver, and lungs. Will be in the system for a very long time
Dosing: 150 mg IVPB, followed by IV infusion 1 mg/min x 6 hrs, then 0.5 mg/min x 18 hrs. May complete 6-10 g load with PO amiodarone once arrhythmia suppressed
Considerations: If arrhythmia does not terminate within 10 min after end of 150mg IV infusion, you can repeat this bolus a second time
Monitoring: Obtain a baseline chest X-ray, pulmonary function tests (including diffusion capacity), TSH, and LFTs when amiodarone therapy is initiated. Repeat history, physical exam, and chest X-ray every 3 to 6 months
Dofetilide
Pro: Safe to use in patients with heart failure
Cons: High risk of torsades, with higher risks if medication is not adjusted for renal function. Therefore, patients need to be admitted to the hospital during the first 3 days of initiation to monitor the QTc.
Dosing: Dependent on renal function. With normal renal function, initial dosing is 500 mcg twice daily (maximum dose: 500 mcg twice daily).
Considerations:
QTc interval should be measured 2 to 3 hours after the first 5-6 doses
For any QTc prolongation >15% or >500ms, dose adjustments must be made
If there is too much prolongation, this may preclude the patient from getting this medication.
Monitoring: Must get EKG, BMP, Mg, and Phos every 3-6 months after administration to monitor QTc, Cr, and electrolytes.
Ibutilide
Dosing: IV infusion 0.01 mg/kg over 10 min (weight < 60 kg) or 1 mg/kg over 10 min (weight ≥ 60 kg)
Considerations:
Acute chemical cardioversion only, not indicated for chronic maintenance therapy
Discontinue as soon as arrhythmia terminates or marked QTc prolongation occurs
Do not use in patients with hemodynamic instability
Give pre-and post-infusion IV magnesium to reduce TdP risk (suppresses early after-depolarizations)
Monitoring:
Pre-infusion Mg level (goal ≥ 2 mmol/L)
Requires continuous ECG during infusion AND at least 4 hours post-infusion due to high risks of Torsades. Make sure patient does not have hypokalemia or hypomagnesemia as this increases torsades risk!
Have crash cart at bedside
Sotalol: Beta-blocker that helps to slow heart rate and AV conduction, as well as prolong atrial and ventricular action potentials
Cons: High risk of torsades. Patients need to be hospitalized during initiation of this drug due to potential QTc prolongation
Dosing: Dosing is renal dependent. For patients with normal renal function, start with 80mg BID. If this dose does not prolong QTc >500 after 3 days, can increase up to 160mg BID
Considerations:
Should NOT be used in patients with HFrEF (EF<40%) as they are most likely also taking an additional AV nodal blocker (i.e. a beta blocker) and this can cause brady or tachy arrhythmias.
QTc interval should be measured 2 to 3 hours after the first 5-6 doses. For any QTc prolongation >15% or >500ms, dose adjustments must be made. If there is too much prolongation, this may preclude the patient from getting this medication.
Monitoring: Must get EKG, BMP, Mg, and Phos every 3-6 months after administration to monitor QTc, Cr, and electrolytes.
Class IV: block L-type calcium channels to delay AV nodal firing
Non-dihydropyridine Calcium Channel Blockers (diltiazem, verapamil)
Pros:
Lower incidence of patient discomfort (dyspnea, chest tightness, flushing)
2017 Cochrane review showed similar conversion rates to NSR compared to adenosine, without significant differences in adverse drug reactions
Con:
As these are negative chronotropic agents, they should be used with caution in patients with acute heart failure.
May potentially be associated with more hypotension
Slower onset (3-5 min)
Longer duration of action (2-5 hrs) and not preferred in patients who are hemodynamically unstable
Dosing:
Diltiazem: IV bolus 0.25 mg/kg (~20 mg) over 2 min, may repeat 0.35 mg/kg (~25 mg) IVP at 15 min
Verapamil: IV bolus 2.5-5 mg over 2 min, may repeat with 5-10 mg at 15 min
Class V:
Digoxin: Stimulates the vegas nerve and causes AV node inhibition
Pro: Used for patients who have afib whose rates are not controlled on other agents. The positive inotropic properties make it advantageous for HFrEF patients as it has minimal impact on blood pressure
Con: Toxicity can occur even at therapeutic levels if patients develop AKIs or hypokalemia. Has a VERY narrow therapeutic index (<2 ng/ml)
Dosing: 0.25 to 0.5 mg once; repeat doses of 0.25 mg every 6 hours to a maximum of 1.5 mg over 24 hours. For more specific weight based dosing, you can visit https://clincalc.com/Digoxin/
Considerations: Look out for digoxin toxicity! Symptoms include nausea, vomiting, visual disturbances (yellow or blurred vision), and lethargy. Patients can also develop arrhythmias, such as paroxysmal atrial tachycardia, all types of AV block, premature ventricular contractions (PVCs), ventricular tachycardia, and ventricular fibrillation.
How’d we do?
The following individuals contributed to this topic: Stephanie Dwyer, PharmD, Jinjoo Chung, PharmD
Resources
Loscalzo, J. (2022). Harrison's principles of internal medicine, twenty-First Edition (vol. 1 & vol. 2). McGraw-Hill Education.
Chiu, A., Kasper, M., Rimmer, J., Donnelly, M., Chen, Y., Chau, C., Sidow, L., & Ash, A. (2017). Remote Management of Atrial Fibrillation: A case report. Clinical Practice and Cases in Emergency Medicine, 1(3), 242–245. https://doi.org/10.5811/cpcem.2017.4.33539
Sabatine, M. S. (2023). Pocket medicine: The Massachusetts General Hospital Handbook of Internal Medicine. Wolters Kluwer.
Flautt, T., & Valderrábano, M. (2021). Recent clinical trials in atrial fibrillation. Current Opinion in Cardiology, 36(6), 798–802. https://doi.org/10.1097/hco.0000000000000914
Dobariya V, Ezeh E, Suliman MS, Singh D, Teka S. Unusual Presentation of Atrial Flutter With Slow Ventricular Response. Cureus. 2021 Jun 21;13(6):e15801. doi: 10.7759/cureus.15801. PMID: 34306869; PMCID: PMC8294030.
Nesheiwat Z, Goyal A, Jagtap M. Atrial Fibrillation. [Updated 2022 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526072/
Mayo Foundation for Medical Education and Research. (2021, October 19). Atrial fibrillation. Mayo Clinic. Retrieved May 1, 2023, from https://www.mayoclinic.org/diseases-conditions/atrial-fibrillation/symptoms-causes/syc-20350624 - Image.
YouTube. (2022). Telemetry Tips - Atrial Flutter, Atrial Tachycardia. YouTube. Retrieved May 1, 2023, from https://www.youtube.com/watch?v=BbLYOcgdPb0.
YouTube. (2014). Intro to Ekg Interpretation - Practicing Tachyarrhythmia Identification. YouTube. Retrieved May 1, 2023, from https://www.youtube.com/watch?v=NULY6Ecj6gA.
Organization, Healio, & ImageObject. (2017, August 2). Left atrial appendage thrombus. Left Atrial Appendage Thrombus | Learn the Heart. Retrieved May 1, 2023, from https://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/atrial-appendage-thrombus Image.
Wikimedia Foundation. (2023, January 30). Atrial flutter. Wikipedia. Retrieved May 1, 2023, from https://en.wikipedia.org/wiki/Atrial_flutter- Image.
Identifying and treating atrial fibrillation (AFIB or AF). ACLS, PALS, and BLS Certification Online. (n.d.). Retrieved May 1, 2023, from https://www.aclsonline.us/rhythms/atrial-fibrillation/ -Image.
Martin, P. (2018, December 12). Atrial flutter. ACLS Wiki. Retrieved May 1, 2023, from https://www.proacls.com/wiki/ekg-rhythms/atrial-flutter/ - image.