Case Presentation:
You are on overnight when a Rapid Response is called for tachycardia on a 56 year old female with PMH of HFpEF, HTN, DM, CKD3, and obesity who is currently being treated for osteomyelitis. When you get to the room, the patient looks tachypneic and uncomfortable, but she is otherwise alert and oriented with warm extremities. You get the following EKG:
Triage Vitals:
HR: 180s BP: 98/69 SpO2: 95% on room air. RR: 30
Ask Yourself:
How do you interpret this EKG?
What is your approach to figuring out what rhythm this patient is in?
How do you treat this rhythm?
Background on Tachycardias:
AVNRT: atrioventricular nodal reentry tachycardia
AVRT: atrioventricular reentry tachycardia
Pro Tip:
Remember to look at telemetry! This can allow you to see what the onset and end of the tachycardia looks like, which can help you determine the underlying rhythm. Plus, you can see if the rhythm was abrupt (more likely AVRT, AVNRT, AT) or if it has been gradually getting faster (i.e. sinus tachycardia)
Approaching an SVT:
Is the patient stable? If unstable (i.e. hypotension, alerted, or respiratory distress), shock!
Is this a narrow or wide complex tachycardia?
Get an EKG! Do you see P waves?
*If yes, do each of the P waves match up with a QRS? If there are more Ps to QRSs, think atrial tachycardia (AT)!
Look at the RP interval (more info on future slides!)
If yes, do each of the P waves match up with a QRS? If there are more Ps to QRSs, think atrial tachycardia (AT)!
If no, you’ll need to slow down the rhythm! Try first with vagal maneuvers followed by adenosine if that does not work.
Make sure the patient is hooked up to a continuous EKG so you can capture the rhythm!
You can also look at telemetry to help determine what the onset and end of the rhythm looked like.
Atrial Tachycardia (AT)
This figure shows a new focus within the atrium that is propagating the rhythm (shown in purple) rather than the P wave originating from the sinus node (pictured in yellow)
AT is due to at least one additional focus in the atrium that sends signals to the atrioventricular (AV) node (see associated image).
Clues that you are dealing with AT:
The AT P waves may look different from the native P wave (as seen the associated EKG)
Sometimes, not all P’s conduct to the ventricles; meaning, there can be more P’s than QRS (i.e. 2:1, 3:1, etc).
The termination of the AT usually does NOT end with a P wave (as seen in figure 4). The reason for this is due to the fact that it is very unlikely that the ectopic focus stops firing and there is a spontaneous block of the AV node both at the same time.
Atrioventricular Nodal Reentry Tachycardia (AVNRT)
AVNRT is a supraventricular tachycardia that occurs due to a re-entry circuit within or around the atrioventricular (AV) node.
Figure A shows how the signal will come from the sinus node to then activate the AV node (green arrow). The signal will pass through both the fast (purple) and slow (pink) pathways. Only the signal from the fast pathway goes through to the common pathway (maroon) because the slow pathway gets blocked by the fast pathway.
Figure B: Since the fast pathway has a longer refractory period than the slow pathway, only the slow pathway will be available to transmit the signal if a premature atrial contraction (PAC) occurs. In this figure, notice how a PAC (blue) can only activate the slow pathway because the fast pathway is in its refractory period (noted by the dashed purple lines).
Figure C shows how the activation from the slow pathway then activates the fast pathway in a retrograde fashion. When this happens, it creates a AVNRT.
Note: There are many iterations of this phenomena, such as slow-fast (shown and most common), fast-slow, and sometimes even slow-slow.
The figure above demonstrates what AVNRT would look like on an EKG.
In A, you can see a normal sinus p wave (green) going through the fast pathway (purple) to activate the Bundle of His for ventricular contraction that creates a QRS (maroon).
B shows how a PAC (blue) activates the slow pathway (pink) since the fast pathway is refractory (illustrated by the dashed purple lines). Note how the PR interval of the slow pathway is longer than that of the fast pathway.
Finally, C demonstrates how the PAC going down the slow pathway creates the re-entry circuit of AVNRT. See how the slow pathway (pink) activates the fast pathway (purple) on the top picture. The fast pathway then travels in a retrograde fashion (creating a retrograde p wave, shown in purple) that then activates the slow pathway. As the fast and slow pathway continue to activate each other, this creates the AVNRT re-entry circuit.
Atrioventricular Reentry Tachycardia (AVRT)
In AVRT, the accessory pathway creates the circuit that allows for the tachycardia. The accessory pathway(s) can be located on the right side, left side, or both sides of the heart. The pathway(s) can go antegrade, retrograde, or both antegrade and retrograde (as demonstrated in the figure above). The most well-known AVRT is Wolf-Parkinson White (WPW), which is famous for its delta wave that shortens the PR interval and causes slurring of the R wave. In the figure below, you can see how the combination of the normal beat (green) plus the antegrade accessory pathway (purple) combine to create the delta wave commonly seen in WPW.
Since the normal sinus beat has to go through the AV node, it may get slowed down while the accessory pathway does not. The morphology of the QRS will depend on which pathway activates the His-Purkinje system first. If the accessory pathway is faster, it will have more of an impact on the QRS and the delta wave will be more prominent. However, if the normal pathway through the AV node is faster than the accessory pathway, the delta wave may be be small or even absent.
How to differentiate the different SVTs:
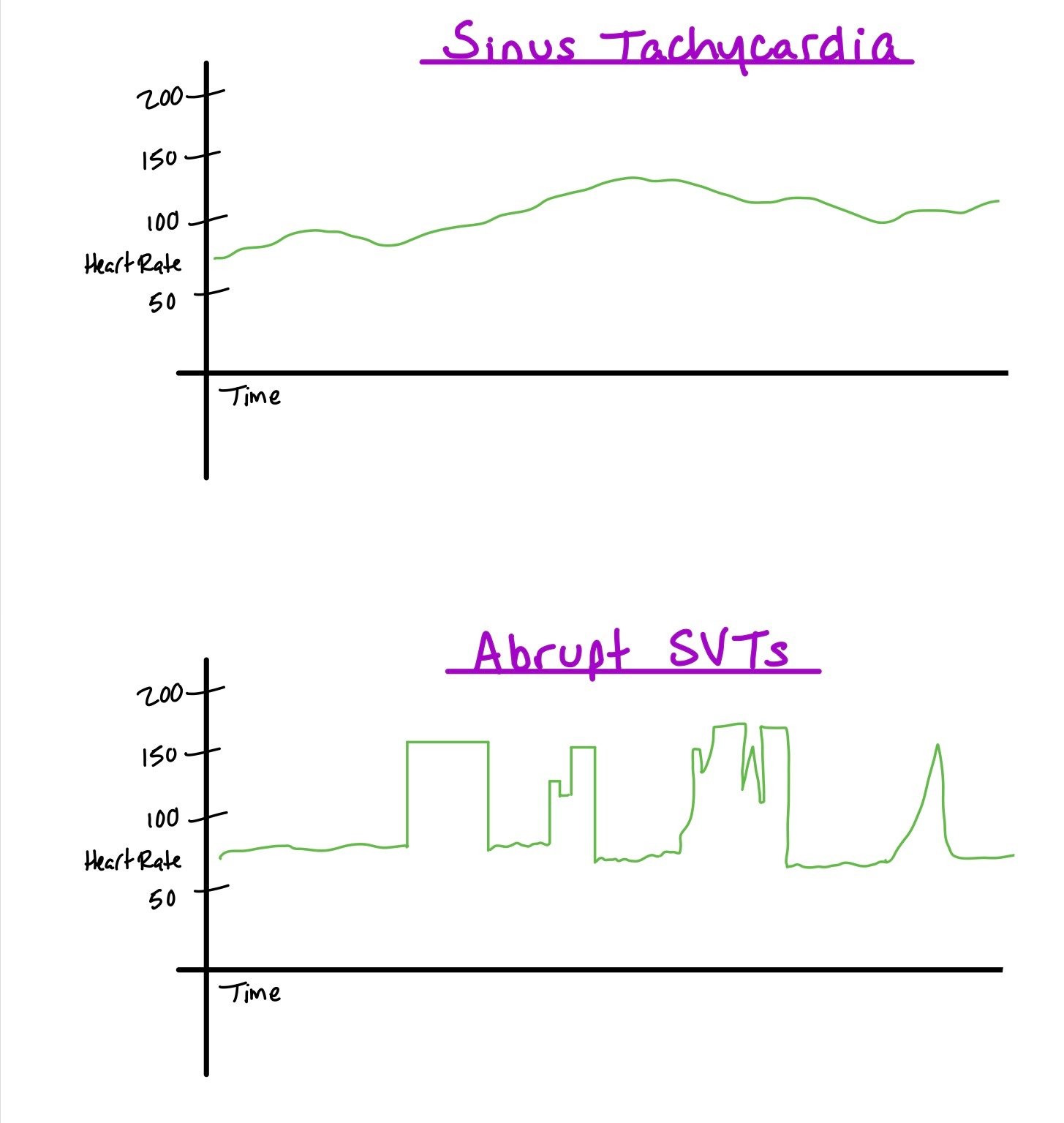
Pay attention to how the tachycardia started and stopped Remember that atrial tachycardia does not usually end with a non-conducted p wave! Also, many times AVRT and AVNRT will start suddenly (unlike sinus tachycardia which is a gradual tachycardia), so looking at the graphic trends (i.e. the heart rate vs time graph) can be very helpful. In the figure to the right, you can see the sudden rise and fall of the heart rate, which is very indicative of AVRT and AVNRT.
Look at P wave morphology and atrial to ventricular activation Look to see if the p wave of the tachycardia looks like similar to baseline. If not, the tachycardia may not be originating from the sinus node. Also remember, atrial tachycardia may have more A to V activity (i.e. more p waves than QRS complexes).
RP Interval This is one of the most important things to look at. Here, we look at the interval from the upsloping of the R wave to the start of the P wave (which may sometimes be inverted). Figure 9 shows the different lengths, known as short, mid-ranged, and long RP.
Response to Adenosine When giving adenosine, it is important to get a continuous EKG. The idea is to get an EKG when the heart rate slows down enough in order for you to distinguish the RP interval. In general, AVNRT and AVRT are responsive to adenosine. Many types of AT are resistant to adenosine!!
Response to Adenosine
Adenosine becomes an important tool because it can terminate the arrhythmia or slow down the AV response.
Sometimes with AVNRT, you cannot see the retrograde p waves during the tachycardia. However, the rhythm will terminate with adenosine.
When patients have orthodromic AVRT, AKA Wolf Parkinson White, you might not be able to see the delta wave during the tachycardia. When the patient goes back into sinus rhythm, the delta wave will appear when you get a signal from both the sinus node and the accessory pathway.
For AT, the adenosine slows down the AV node. When this happens, you can see the atrial activity as the atria is still firing.
Similar to AT, atrial flutter can be distinguished with adenosine as you will be able to see the flutter waves after the adenosine is pushed.
What do you think would happen if you gave adenosine to someone who has ventricular tachycardia? Nothing! The VT continues, and perhaps blocks VA conduction.
Pharmacotherapies:
Adenosine: AV nodal blocker; interrupts re-entry pathways through AV node
Dose: 6 mg rapid IVP x 1, may repeat 12 mg x 2 (some data to support higher 18 mg as 3rd dose)
Administration tips:
Give via 2-way stopcock (adenosine first, quickly followed by NS flush) OR dilute adenosine with 15-20 mL NS into a single syringe to reduce administration delays/errors
Administer into most proximally available peripheral IV
Benefits: Very short half-life (<10 sec)
Contraindication(s):
Very well tolerated
Non-DHP Calcium Channel Blockers: block L-type calcium channels to delay AV nodal firing
Reasonable first line therapy for SVT without pre-excitation
Pros:
Requires less coordination for administration than adenosine
Lower incidence of patient discomfort (dyspnea, chest tightness, flushing) compared to adenosine
2017 Cochrane review showed similar conversion rates to NSR compared to adenosine without significant differences in adverse drug reactions
Cons:
May potentially be associated with more hypotension
Slower onset (3-5 min) compared to adenosine. Longer duration of action (2-5 hrs) compared to adenosine. Not preferred in unstable patients
Diltiazem:
Dose: IV bolus 0.25 mg/kg (~20 mg) over 2 min, may repeat 0.35 mg/kg (~25 mg) IVP at 15 min
Verapamil:
Dose: IV bolus 2.5-5 mg over 2 min, may repeat with 5-10 mg at 15 min
Procainamide: Class IA antiarrhythmic (blocks Na channels; decreases conduction velocity, prolongs QTc)
***Recommended agent in SVT w/ known accessory pathways
Dose: IV 10-17 mg/kg admin at 20-50 mg/min (or in increments of 100 mg Q5min up to 17 mg/kg)
If starting maintenance dosing (IV 1-5 mg/min or PO 500-1250 mg Q6h) after arrhythmia suppression, requires renal/hepatic dose adjustments and CBC monitoring
High risk for QTc and QRS prolongation
Stop infusion if arrhythmia terminates during bolus, pt becomes hypotensive, or QTc/QRS widens >50%
Back to the Case…
Ask Yourself Answer Key:
1. How do you interpret this EKG?
If you look closely, you can see hidden P waves that fall within the T wave. Once you identify where the p waves are, you can determine the length of the RP interval (i.e. the distance between the R and the P wave). Shorter RP intervals are more likely to be AVNRTs, while longer intervals tend to identify AVRTs. Regardless, these patients needs adenosine and an EP study to determine the exact reason for the SVT and to fix it.
2. What is your approach to figuring out what rhythm this patient is in?
It’s important to ensure the patient has a continuous EKG strip running when they vagal or when adenosine is given, so we can see what the underlying rhythm is when the SVT slows down or how it terminates. You can also look at or call telemetry to see what the graphic trends of the patient’s heart rates are. Any time the SVT starts and ends abruptly, this is concerning for AVRT or AVNRT (vs sinus tachycardia, afib, aflutter). Remember–adenosine is both diagnostic and therapeutic.
3. How do you treat this rhythm?
There are multiple oral options for treating the rhythm, such as AV nodal blockers to interrupt re-entry pathways (adenosine), delay AV nodal conduction (non-DHP CCB), or blocking Na channels and decreasing conduction velocity (procainamide). Plus, CCB and beta blockers can also decrease the amount of PACs so that the arrhythmia is not reactivated. Regardless, definitive treatment is usually with ablation of the slow pathway (in AVNRT), accessory pathway (in AVRT), or ectopic focus (AT).
Further Learning:
Resident Responsibilities
When you first walk into a patient’s room who is in SVT, make sure they are connected to the monitor and have the EKG machine running.
If the patient is not stable, shock!
If the patient is stable, call telemetry to see if this tachycardia started abruptly. If so, you are most likely dealing with an SVT, like AVNRT, AVRT, or AT. Remember, the last thing you want to do is shock sinus tachycardia!
Start with vagal maneuvers. If this does not work, you can push adenosine (1st- 6mg, 2nd- 12mg, 3rd- 12mg). When pushing the adenosine, make sure the patient’s arm is raised and that the adenosine push is followed IMMEDIATELY by a saline push because the half life of adenosine is so short.
Make sure the EKG is running when the adenosine is pushed!
Attending Pearls
Sometimes looking at old EKGs can help clue you into accessory pathways (such as WPW).
Make sure to get an EKG before, during, and after the arrhythmia terminates! Note! Sometimes SVTs can look like ventricular tachycardia if the patient has a baseline bundle branch block, SVT with aberrancy, or a particular type of accessory pathway!!
For vagal maneuvers, you can ask the patient to bear down or blow into a syringe. If they are unable to do either, you can try laying the patient back and lifting their legs up in the air, as this involves less patient cooperation.
If adenosine 12mg does not work, you can try 18mg. If that does not work and the patient is not stable (i.e. AMS, hypotensive), shock. However, if the patient is stable, you can always try a different agent, such as a non-DHP CCB or procainamide.
Further Reading / Learning:
Dr. Joshua Coopers, Temple University, SVT series:
WPW Explanation and Treatment
EKG reading: How the QRS is made
Dr. Stacy Wasserman, Emory University: SVT
How’d we do?
The following individuals contributed to this topic: Victor Qiao, MD, Isaac Whitman, MD, Stephanie Dwyer, PharmD, Jinjoo Chung, PharmD
Resources
Padanilam, Benzy J., et al. “Differentiating Atrioventricular Reentry Tachycardia and Atrioventricular Node Reentry Tachycardia Using Premature His Bundle Complexes.” Circulation. Arrhythmia and Electrophysiology, vol. 13, no. 1, 2020, pp. e007796–e007796, https://doi.org/10.1161/CIRCEP.119.007796.
Kotadia, Irum D., et al. “Supraventricular Tachycardia: An Overview of Diagnosis and Management.” Clinical Medicine (London, England), vol. 20, no. 1, 2020, pp. 43–47, https://doi.org/10.7861/clinmed.cme.20.1.3.
Mani, Bhalaghuru Chokkalingam, and Behzad B. Pavri. “Dual Atrioventricular Nodal Pathways Physiology: A Review of Relevant Anatomy, Electrophysiology, and Electrocardiographic Manifestations.” Indian Pacing and Electrophysiology Journal, vol. 14, no. 1, 2014, pp. 12–25, https://doi.org/10.1016/S0972-6292(16)30711-2.
Ding, Wern Yew, and Saagar Mahida. “Wide Complex Tachycardia: Differentiating Ventricular Tachycardia from Supraventricular Tachycardia.” Heart (British Cardiac Society), vol. 107, no. 24, 2021, pp. 1995–2003, https://doi.org/10.1136/heartjnl-2020-316874.
FERGUSON, John D., and John P. DIMARCO. “Contemporary Management of Paroxysmal Supraventricular Tachycardia.” Circulation (New York, N.Y.), vol. 107, no. 8, 2003, pp. 1096–99, https://doi.org/10.1161/01.CIR.0000059743.36226.E8.
Ganz, Leonard I., and Peter L. Friedman. “Medical Progress: Supraventricular Tachycardia.” The New England Journal of Medicine, vol. 332, no. 3, 1995, pp. 162-, https://doi.org/10.1056/NEJM199501193320307.