Case Presentation:
A 64 year old male with PMHx of MI s/p DES x2 ~1 month ago for a STEMI, paroxysmal atrial fibrillation (AF), HTN, DM2, HLD presents to the ER for two days of melena. The patient’s medications include apixaban and clopidogrel for the recent DES placement and his history of AF.
Ask Yourself:
Questions:
1. What interventions do you want to provide to the patient immediately?
2. Which interventions can be delayed but should be completed in the next 24 hours?
3. Are there any services you want to consult?
4. Are there any medications you would like to change or hold?
5. If any medications are held, when would it be appropriate to re-initiate these medications?
Vitals: Afebrile, HR 110s-120s, BP 110s/70s, saturating >95% on room air.
Labs: CBC with hgb 7 (baseline 13), BMP with BUN of 70 and Cr 2.3 (baseline 1.4), lactate 2.5, HS troponin of 48→370.
EKG: Normal sinus rhythm with rates in the 110s. Normal axis / intervals. No acute ST elevations / depressions. Q waves in the precordial leads. Notable nonspecific T wave inversions in III, V4, V5, and V6 (not previously seen)
On exam, the patient appears slightly pale, but otherwise non-toxic appearing. He is tachycardic with no murmurs appreciated. Lungs are clear to auscultation bilaterally. Abdomen is soft, non-tender, and non-distended. Digital rectal exam shows bright red blood per rectum.
Background:
Firstly, what do the guidelines say?
For Dual Antiplatelet Therapy (DAPT):
Guidelines state that patients who have had PCIs due to ACS should have 12 months of DAPT with aspirin + P2Y12 inhibitor. After 12 months, they should continue on only one of these medications (usually aspirin) indefinitely.
When patients receive stents in non-ACS settings, they should be on 6 months of DAPT. After 6 months, they should be continued on only one of these medications (usually aspirin) indefinitely.
If a patient has a history of AF or venous thromboembolism and is already on a direct oral anticoagulants (DOAC) prior to the PCI (whether in the setting of ACS or non-ACS), they should be continued on the DOAC + the P2Y12 inhibitor. After the respective 12 or 6 months, they should be continued on the DOAC indefinitely.
ACG guidelines for GI bleed while on DAPT recommend AGAINST holding aspirin in the setting of GI bleeding. If aspirin was held, aspirin should be resumed on the day hemostasis is endoscopically confirmed (on the day of EGD/colonoscopy).
The rationale is that aspirin irreversibly blocks platelet COX-1 for 7-10 days (length of platelet life)
ALL PATIENTS WITH GI BLEED SHOULD BE ON HIGH-DOSE PPI INDEFINITELY.
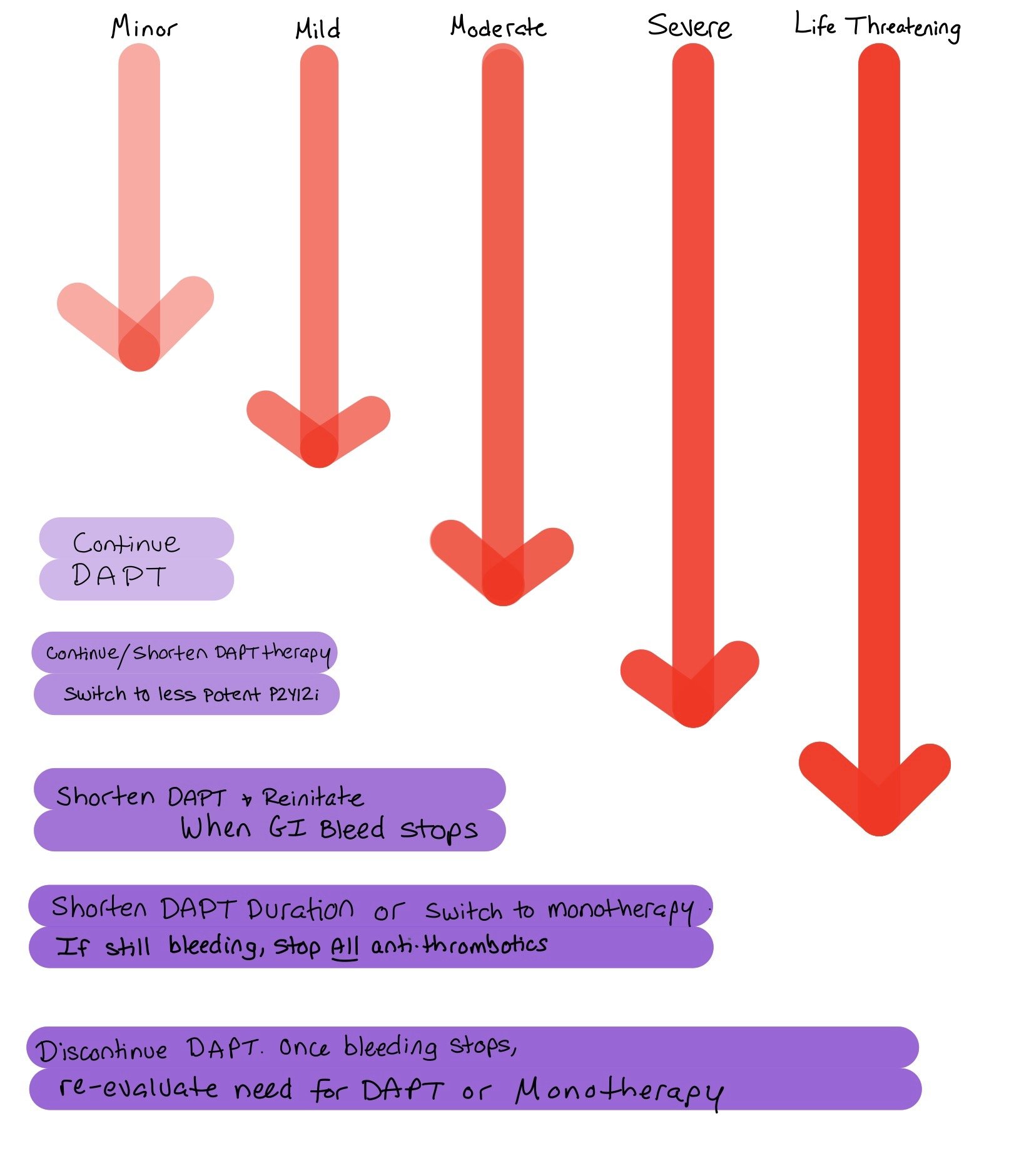
Risk Stratification:. The European Society of Cardiology has the following recommendations
Trivial GI bleed (bleeding not requiring medical intervention)
Continue DAPT therapy
Mild GI bleed (bleeding requiring medical attention w/o hospitalization)
Continue DAPT
Consider shortening DAPT or switching to less potent P2Y12 inhibitor (clopidogrel is least potent)
Moderate GI bleed (bleeding associated with significant blood loss (>3g/dL hgb) but hemodynamically stable
Consider decreasing from DAPT to monotherapy
Reinitate DAPT when safe (endoscopically bleed has stopped)
Severe GI bleed (bleeding assoaicted w/ severe blood loss (>5g/dL hgb) but hemodynamically stable
Consider decreasing from DAPT to monotherapy (preferably continue P2Y12 as it causes less irritation to GI mucosa)
If bleeding persists despite treatment, consider stopping all antithrombotics
Once bleeding is controlled, re-evaluate need for DAPT (Precise DAPT) and re-initiate
If DAPT restarted, consider shortening DAPT duration or using less potent P2Y12 inhibitor
Life-threatening GI bleed (bleeding putting patient’s life at risk)
Discontinue DAPT
Once bleeding has ceased, re-evaluate need for DAPT or monotherapy (preferably with P2Y12 inhibitor)
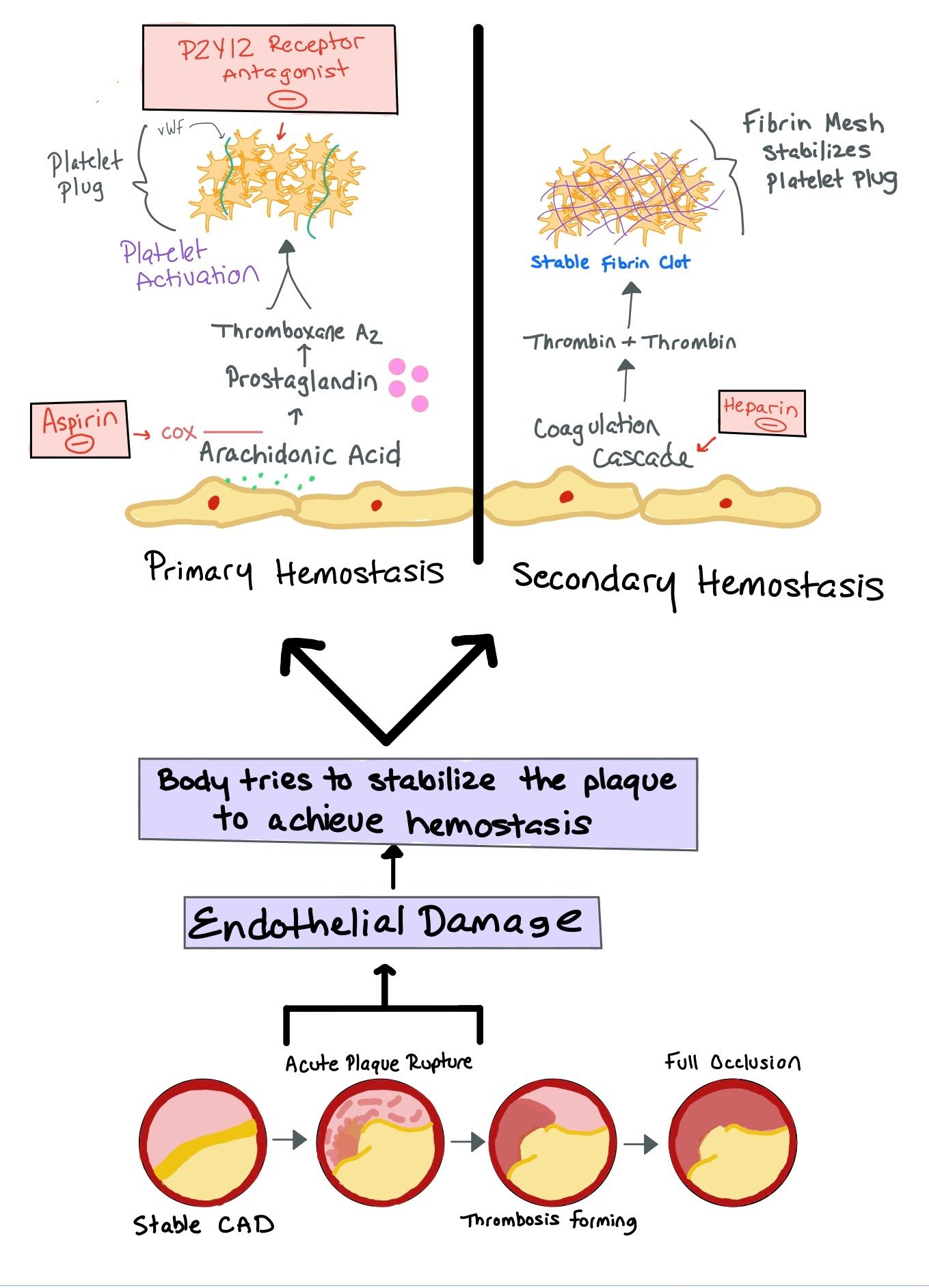
Pathway for PCI
This figure shows how the P2Y12 inhibitors (i.e. Clopidogrel, Ticagrelor, Prasugrel) bind to the P2Y12 receptor to prevent platelet activation. Similarly, Aspirin inhibits COX 1 and 2, ultimately preventing additional platelet activation..
Secondly, what does the art of medicine say?
Decisions on holding DAPT should occur on a case-by-case basis. In general, efforts should be made to continue antiplatelet therapy unless bleeding is life threatening (especially if PCI was recent and in the setting of ACS). It is reasonable to change from DAPT to monotherapy at 6 months for PCI in ACS and at 3 months for PCI in non-ACS.
In-stent thrombosis (IST) is generally a total occlusion of a coronary stent that was placed. The use of DAPT is to prevent IST. The highest risk for IST is within the first month, making DAPT essential during this time. IST within 1-3 months is also very common
If a patient develops IST, this presents similarly to ACS and often has ST elevations on the EKG. Similarly to STEMIs, IST CAN BE DEADLY.
Additionally, in specific scenarios, stopping DAPT after 1 month is possible. Within the 1st month, there is the greatest risk of IST
2025 ACS Updates
P2Y12 Inhibitors: When thinking about P2Y12 inhibitors, there are three main medications: ticagrelor, prasugrel, and clopidogrel. When patients present with ACS, the guidelines recommend ticagrelor or prasugrel as they had decreased major adverse cardiac events (MACE) and stent thrombosis as compared with clopidogrel.
The figure above from the updated 2025 ACS Guidelines shows which P2Y12 Inhibitor is preferred when patients come in with ACS, CABG, have not had any invasive intervention, or were initially treated with fibrinolytic therapy.
The above figure, from CORE IM 5 Pearls on Dual Anti-platelet Therapy helps to show the difference between the 3 main P2Y12 Inhibitors.
When thinking about length of anti-platelet therapy, the guidelines have changed in regards to patients who are at higher bleeding risk. Generally speaking, the guidelines prefer 12 of months DAPT therapy when patients present with ACS. If they are very high bleeding risks, PPI should be used. Additionally, they can potentially continue DAPT therapy for 1 month post-PCI and continue ticagrelor monotherapy after 1 month. See the chart below for more details.
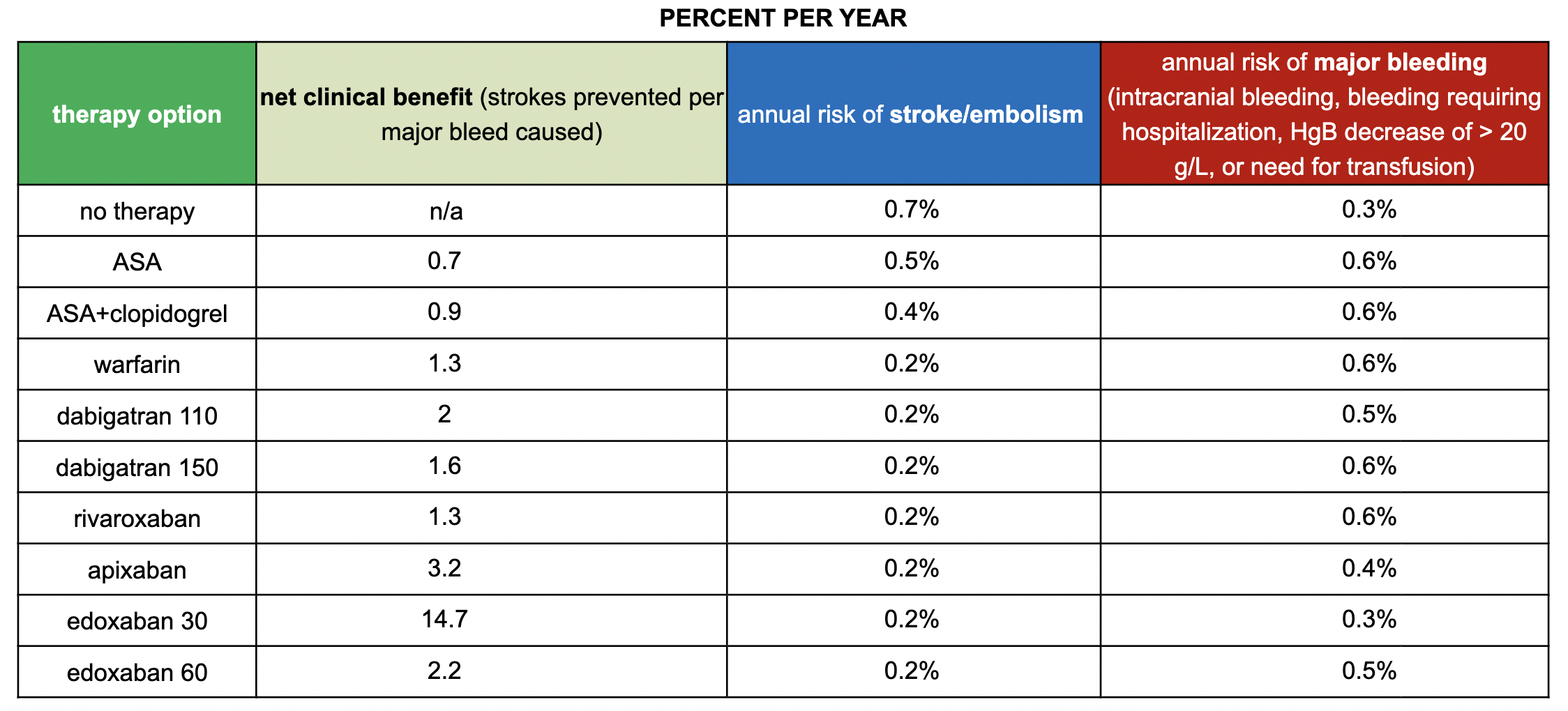
SPARCtool - Stroke Prevention in Atrial Fibrillation Risk Tool
This scoring system can be used to help estimate the risks and benefits of antithrombotic therapy in patients with chronic nonvalvular atrial fibrillation
In the first section, you fill out the patient’s CHA2DS2-VASc Score, which helps determine the patient’s risk for developing a stroke, and the HAS-BLED Score, which shows the patient’s risk for bleeding.
Next, you pick the specific agent the patient is taking.
With this information, the calculator will help generate the net clinical benefit, annual risk of stroke/embolism, and risk of major bleed for each medication.
What if the patient also has atrial fibrillation (AF)?
All patients with AF are at an increased risk for cardioembolic phenomena due to the concern for clot development in the left atrial appendage (LAA). Anytime a patient develops AF, we must calculate their CHA2DS2-VASc score, which helps us determine their risk for stroke.
The figure shows the LAA and where a clot can form. The higher this score, the greater their chance for developing a cardioembolic phenomena. A risk-benefit conversation regarding the need for anticoagulation to prevent any cardioembolic phenomenon balanced with the risk for bleeding should be had with each patient who has AF. Note: Direct oral anticoagulants (DOACs) like apixaban and xarelto have been shown to be superior and non-inferior to warfarin for treating AF. The only time warfarin should be used is if a patient has moderate-severe rheumatic mitral stenosis or has a mechanical heart valve.
This figure depicts the left atrial appendage and shows where the clot forms within the LAA. Due to each patient’s increased risk for cardioembolic phenomena, you must calculate and document their CHA2DS2-VASc score to assess their risk! Men with scores >2 and women >3 should be considered for anticoagulation!
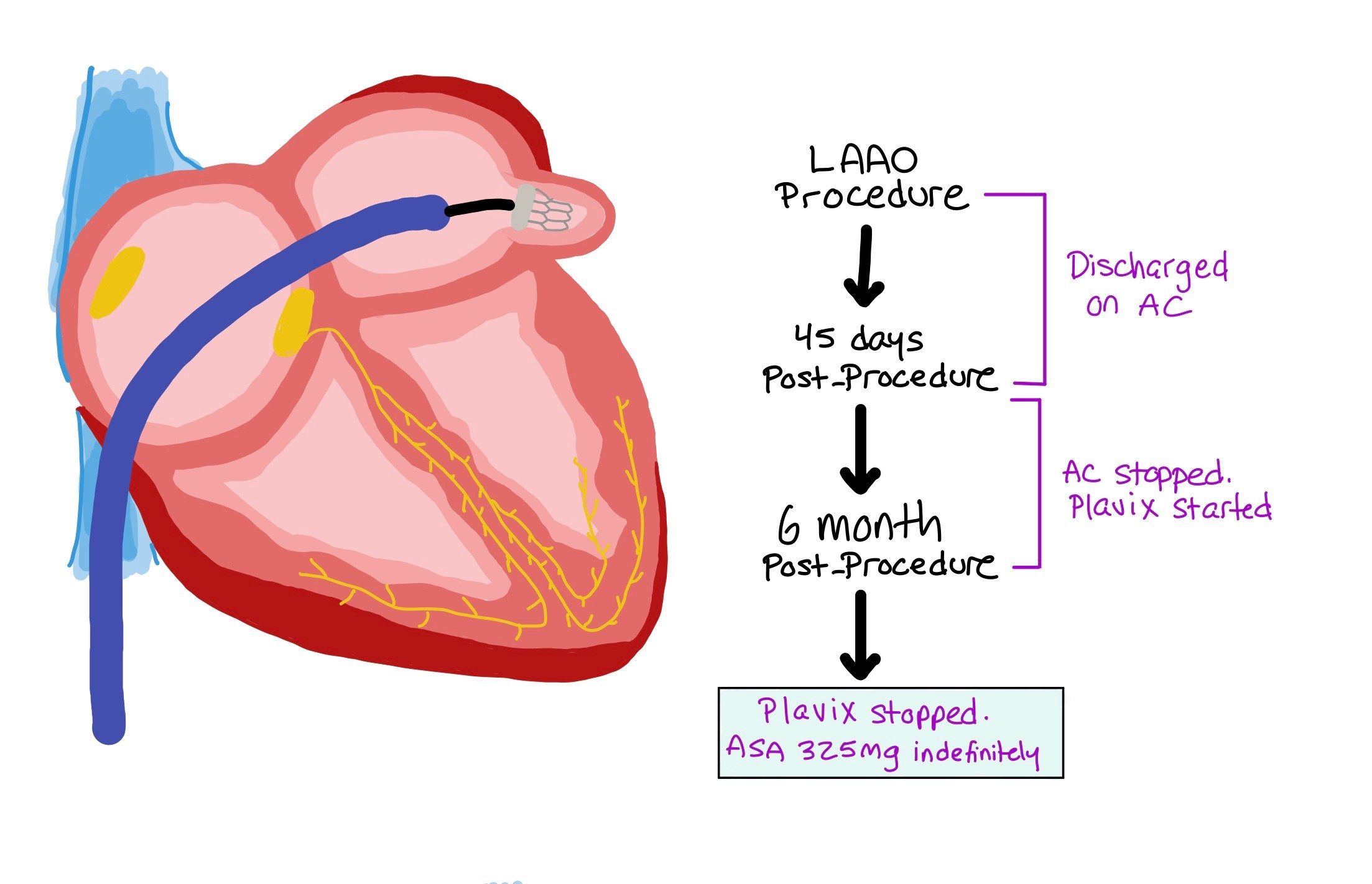
If patients have had a serious bleed in the past while on anticoagulation, they may be candidates for left atrial appendage occlusion (LAAO) with a device called a Watchman. These devices are placed by interventional cardiologists in the left atrial appendage. Over time, the area over the Watchman will epithelialize, in essence closing the left atrial appendage.
NOTE: When patients receive Watchmans, they will be on anticoagulation for the first 45 days, followed by plavix for the next 6 months, and will ultimately be on aspirin monotherapy indefinitely.
Back To The Case:
1. What interventions do you want to provide to the patient immediately?
IV PPI, Type and screen→ pRBC transfusion, consider holding one of the anti-platelet agents: either the P2Y12 inhibitor or aspirin
2. Which interventions can be delayed but should be completed in the next 24 hours?
Endoscopy (studies show that for upper GI bleed, endoscopy between 6-24hrs is appropriate. Additionally, resuscitating the patient so they are hemodynamically stable prior to endoscopy is essential),
3. Are there any services you want to consult?
Consult GI and cardiology
4. Are there any medications you would like to change or hold?
From multiple sources, it appears that history of medical inertia from physicians leads to physicians stopping the P2Y12 inhibitors first and continuing with aspirin monotherapy. However, new evidence from the European Society of Cardiology suggests that P2Y12 inhibitors should be continued because aspirin causes both anti-platelet mechanisms and also disrupts the GI mucosa. The irritation of GI mucosa may be more important for upper GI bleeds than lower GI bleeds.
If the patient is on prasugrel/ticagrelor, consider switching to clopidogrel d/t lower bleed risk. Another thing to consider with ASA, because it irreversibly inhibits platelet aggregation, stopping ASA likely won’t have much of an effect until the life-span of platelets ends (7-10 days)
Guidelines state that 1 year of DAPT therapy is require for PCI in the setting of ACS. The first 3 months are the most crucial for anti-platelet therapy as the risk for in-stent thrombosis is the highest. All patient’s w/ GI bleed should be on PPI indefinitely
5. If any medications are held, when would it be appropriate to re-initiate these medications?
If asa or P2Y12 inhibitor was held, it can be re-initiated if low-risk bleed. If higher risk bleed, consider holding one of them but can be held for a few days but should be restarted. The decision to add both asa and P2Y12 inhibitor is a case-by-case decision, but ideally patient will be on DAPT through at least 3 months.
Further Learning:
Resident Responsibilities
When thinking about duration of DAPT, it is important to know if the stent was placed in the setting of acute plaque rupture (i.e. ACS) or stable angina (i.e supply vs demand issue). Typically speaking, DAPT for ACS is continued for 12 months, while DAPT for stable CAD is continued for 6 months. After this, patients should be continued on monotherapy indefinitely.
In complicated cases where patients have bleeds, patients who had ACS should be continued on DAPT for 6 months, while non-ACS should be continued on DAPT for 3 months.
The reason we continue DAPT post-PCI is to prevent stent thrombosis, which is an ACUTE, deadly thrombosis of the stent (think stent thrombosis, ST elevation— an emergent issue). Stopping DAPT early puts patients at high risk for stent thrombosis as the PCI can still irritate the endothelium and cause acute thrombosis. In contrast, there is in stent restenosis, which is a more chronic issue with intimal proliferation in which the stent slowly gets reclogged. To prevent this, we use drug eluding stents to help prevent cell proliferation and limit in stent restenosis.
Attending and Fellow Pearls
Anytime you are putting patients on anticoagulation or anti-platelets, it is imperative that you tell them warning signs to look out for, such as occult bleeding or melena.
On that point, it is important that you then document that you have had the risk / benefit discussion whether you are starting or stopping these medications.
Whenever you start any anticoagulation or anti-platelet, make sure to document expected duration!
If there’s a question about duration of therapy given severe bleed, always try to make the interventional cardiologist who was involved in the patient’s care aware and to help weigh in on appropriate duration and therapy.
Further Learning
ULTIMATE-DAPT
New data coming out of ACC2024 showing that patients getting a PCI for STEMI may be able to be on 1 month of Ticagrelor and aspirin followed by 11 months of Ticagrelor monotherapy. This decreased bleeding without differences in composite cardiovascular mortality. This data is new, but very exciting!
CORE IM DAPT
https://www.coreimpodcast.com/2021/04/07/5-pearls-on-dual-antiplatelet-therapy/
CORE IM Aspirin for Primary Prevention
https://www.coreimpodcast.com/2022/10/19/mind-the-gap-aspirin-for-primary-prevention/
Progression of GI Injury During Antiplatelet Therapy After Percutaneous Intervention, JAMA
https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2812100
How’d we do?
The following individuals contributed to this topic: Michael Siegel, DO, Sean Tompkins, MD, PhD
Chapter Resources
https://www.giejournal.org/article/S0016-5107(20)30238-8/fulltext
https://www.thieme-connect.de/products/ejournals/pdf/10.1055/s-0034-1393172.pdf
https://www.sparctool.com/
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001038