Case Presentation:
You are admitting a 75 year old male with PMH of HFpEF, aortic stenosis, HTN, DM, HLD, and gout to the CCU for 1 month of progressive shortness of breath over the past few months and new syncopal episode. When getting his history, you find out that he also has been experiencing melena on and off for the past few months. On exam, he has conjunctivae pallor, a loud crescendo decrescendo systolic murmur on right 2nd intercostal space, clear lung sounds, and no abdominal tenderness although his DRE is positive.
Ask Yourself:
1. What is your differential for what is happening with the patient?
2. What labs and imaging would you order?
3. What acute interventions does this patient need?
4. Are there any other interventions you want to perform?
Vitals: Afebrile, HR 90-110s, BP 110s/70s, saturating >95% on room air.
Labs: CBC with hgb 6.5 (baseline 13), BMP with BUN of 70 and Cr 2.2 (baseline 1.4), lactate 3, HS troponin of 500—>490. Ferritin <10. LFTs with elevated total bilirubin, direct wnl. LDH elevated.
EKG: Normal sinus rhythm with rates in the 100s. Normal axis / intervals. No ST elevations/depressions. Notable LVH appreciated. QTc 450.
TTE: Diastolic dysfunction with EF 50-55%; Notable worsening of the patient’s previous aortic stenosis with valve area 1 cm2, mean gradient 45 mmHg, and aortic jet velocity 5 m/s.
Background:
When patients present with both severe aortic stenosis and GI bleed, it is important to recognize that these two syndromes may be connected. If this is the case, the patient may have Heyde’s Syndrome.
Heyde’s Syndrome is a syndrome that is made up of :
Severe Aortic Stenosis
Acquired von Willebrand Syndrome
GI bleed from angiodysplasia
Reasons for Aortic Stenosis:
Congenital: Usually presents with uni-or bicuspid valves. Patients are typically young (<30 years old)
Calcified bicuspid: Age 40-60 years old
Rheumatic heart disease: Age 40-60 years old
Senile degeneration: > 70 years (most common)
Signs and Symptoms of Aortic Stenosis:
Chest pain:
As the aortic stenosis worsens, this causes increased afterload on the left ventricle and increased wall stress. The heart will compensate by undergoing left ventricular hypertrophy. Usually, blood goes from the aorta to the coronaries, which is from a high to low pressure system. As the pressures within the left ventricle increase, there is less of a gradient from the aorta to the left ventricle and it becomes harder for blood to flow into the coronary arteries. As a result, patients may experience angina.
As muscle thickness within the left ventricle increases, there can be an oxygen mismatch, which can also cause anginal symptoms
Syncope
A stenotic aortic valve may impede flow, which may lead to decreased brain perfusion and cause syncope
Dyspnea
A stenotic aortic valve can cause lead to poor perfusion, leading to poor peripheral oxygenation and feelings of fatigue
Overtime, the heart may lose its ability to compensate. When this happens, the EF can decrease, causing patients to experience heart failure symptoms.
The figure above shows an apical five chamber view (i.e. an apical four chamber view of the left atrium, left ventricle, right atrium, and right ventricle with the addition of the aortic valve). When patients have stenotic aortic valves, this will impede blood flow out of the aortic valve. The picture on the right shows the difference between a normal vs stenotic aortic valve when the valve opens and closes.
Physical Exam:
Heart sounds:
Crescendo-decrescendo murmur that may move to the carotids
Lack of S2 when stenosis is severe
S4 due to stiffening of the left ventricle
Slow rising carotid pulse (pulsus tardus) with decreased amplitude (pulsus parvus)
On TTE, you may be able to see the calcified aortic valve. You may also see concentric left ventricular hypertrophy, as the stenosis causes increased afterload in the left ventricle and increased wall stress. Overtime, this can cause diastolic dysfunction due to a stiffer ventricle.
There are measurements on TTE that we look at to measure the extent of the aortic stenosis. Specifically, we look at the aortic jet velocity, the mean gradient, and valve area, and then classify the aortic stenosis as normal, mild, moderate, or severe (Table 1).
Acquired von Willebrand Disease:
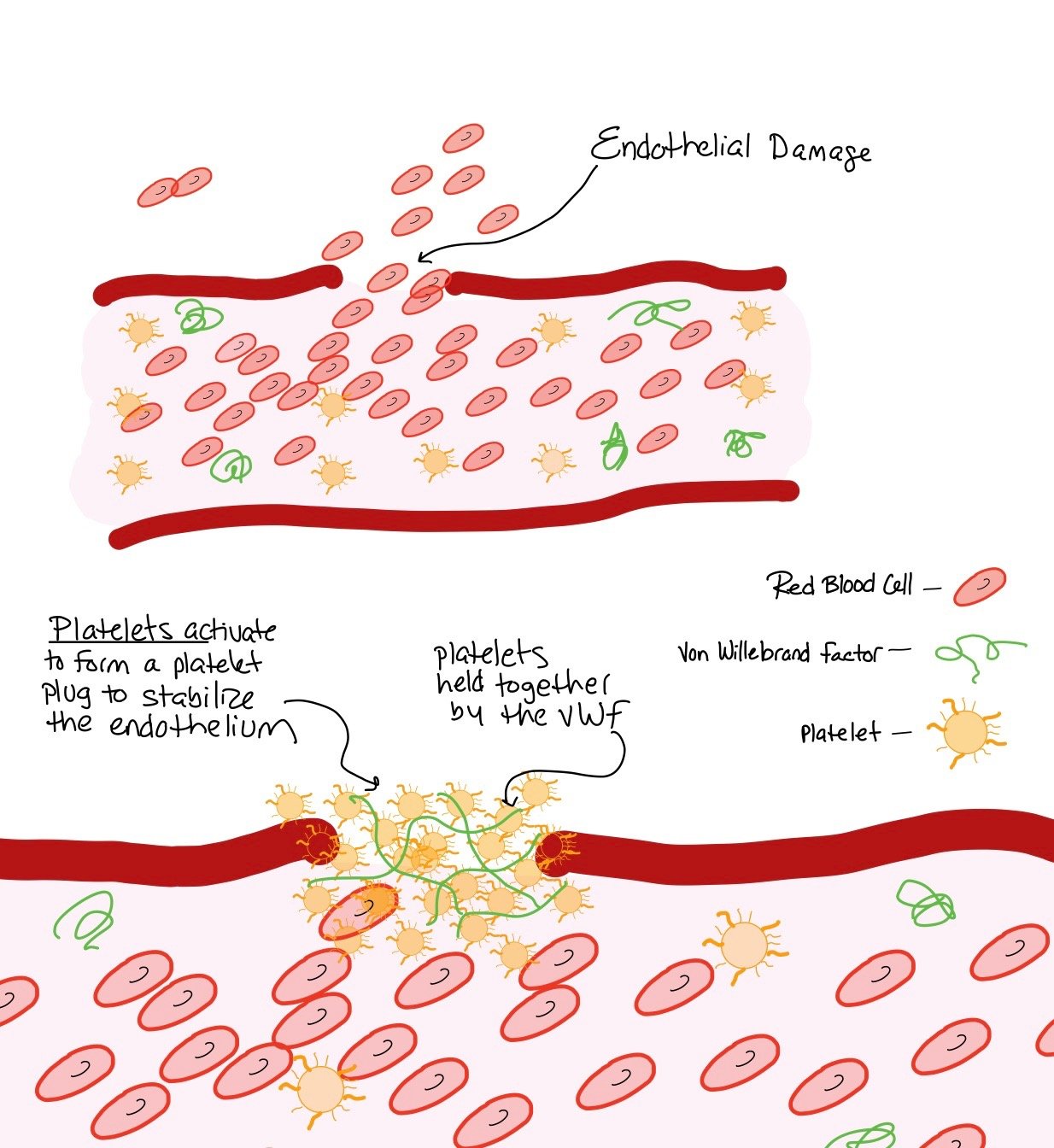
The von Willebrand Factor (vWF) is crucial in maintaining hemostasis by helping to stabilize platelets. Specifically, the vWF acts by mediating platelet adhesion to parts of the endothelium that may be damaged, which allows for platelet aggregation and hemostasis (picture below).
The picture above shows endothelial damage. When this happens, the platelets aggregate together to form a clot and stabilize the endothelium. As pictured, the vWF helps to hold the platelets together, making it an important part of achieving hemostasis.
How does this happen?
When patients have severe aortic stenosis, this can the vWF, a crucial factor in maintaining hemostasis.
When cleaved, the vWF is now more susceptible to being broken up by the ADAMTS-13 protease and thus cannot stabilize platelet mediated hemostasis, making the patient more prone to bleeding.
With multiple VWF fragments, there is also a decrease in clotting factor VIII transport, which indirectly leads to higher bleeding risks.
Additionally, the vWF is also thought to be crucial for suppressing angiogenesis via integrin and vascular endothelial growth factor (VEGF) signaling. Therefore, loss of the vWF not only makes a patient more susceptible to bleeding due to lack of platelet stabilization but also by leading to increased angiogenesis and angiodysplasia.
Picture courtesy of Loscalzo J. “Heyde's syndrome”. N Engl J Med. 2012 Nov
This picture shows how aortic stenosis can cleave the vWF as it goes through the calcific valves. The shear stress that cleaves the vWF and causes it to uncoil and the A2 domain, which allows for the ADAMTS-13 protease to come and cleave the vWF.
Back To The Case:
1. What is your differential for what is happening with the patient?
Anytime patients present with GI bleeds, it is important to keep the differential wide. Most commonly, patients can have peptic ulcer disease (PUD), hemorrhoidal bleed, colon cancer, diverticulosis (especially in elderly), arteriovenous malformations (AVMs), gastritis, angiodysplasia, and, sometimes even Heyde’s Syndrome when severe aortic stenosis is present
2. What labs and imaging would you order?
Start with the basic labs including CBC, CMP, LFTs, PT/INR, and type and screen. However, to further work-up Heyde’s Syndrome, assessment of vWF using the Platelet Function Assay (PFA) and VWF Multimer Assay are recommended. Regarding imaging, TTE should be ordered to evaluate the valve (to grade the aortic stenosis if not known). CTA abdomen and pelvis can be ordered if the patient is actively bleeding to help localize the GI bleed. If the bleed can be localized, Interventional Radiology may be consulted to help embolize the bleed Ultimately, this patient will need both an EGD/Colonoscopy to help gain for source control for the bleed.
3. What acute interventions does this patient need?
The patient needs to be transfused due to his low hemaglobin (<7). Make sure the patient has two large bore IVs in case the bleeding gets worse. Any time you are worried about upper GI bleed, you can start IV PPI. Ultimately, this patient will need a GI consult to determine how soon they need to be scoped.
4. Are there any other interventions you want to perform?
Once the bleed is stabilized, the patient should be evaluated for aortic valve replacement given his severe aortic stenosis. As there is a direct correlation with how the severity of the aortic stenosis and vWF abnormalities, fixing the patient’s valve can help prevent further vWF destruction and hopefully further bleeding events.
Further Learning:
Resident Responsibilities
Any time an elderly patient presents with a GI bleed, always think about Heyde’s as treating the aortic stenosis can help prevent further episodes of bleeding!
Note that even when patients have had their aortic valves replaced (i.e. with transaortic valve replacement, TAVR, or surgical aortic valve replacement, SAVR) they can still get a functional cleaving of the vWF or hemolysis from the valve! In this case, you should test the LFTs, haptaglobin, LDH, and reticulocyte counts to ensure there is no hemolysis occuring!
Further Reading
“Reduction of GI Bleeding in Patients with Heyde Syndrome Undergoing TAVR Implimentation” (Goldstein et al, Circulation, 2022)
https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.122.011848
“Gastrointestinal Angiodysplasia and Aortic Stenosis” (Warkentin, NEJM 2002)
https://www.nejm.org/doi/full/10.1056/NEJM200209123471122
How’d we do?
The following individuals contributed to this topic: Zeel Modi, MD, Sean Tompkins, MD, PhD
Chapter Resources
EC Heyde. Gastrointestinal bleeding in aortic stenosis.N Engl J Med, 259 (1958), p. 196, 10.1056/NEJM195807242590416
Randi AM, Laffan MA, Starke RD. Von Willebrand factor, angiodysplasia and angiogenesis. Mediterr J Hematol Infect Dis. 2013 Sep 02;5(1):e2013060
Aghighi M, Taherian M, Sharma A. Angiodysplasia. 2022 Aug 22. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 31747184.
Lourdusamy D, Mupparaju VK, Sharif NF, Ibebuogu UN. Aortic stenosis and Heyde's syndrome: A comprehensive review. World J Clin Cases. 2021 Sep 6;9(25):7319-7329. doi: 10.12998/wjcc.v9.i25.7319. PMID: 34616798; PMCID: PMC8464459.
Theis SR, Turner SD. Heyde Syndrome. 2022 Jul 11. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan–. PMID: 31869089.
Hillegass WB, Limdi NA. Valvular Heart Disease and Acquired Type 2A von Willebrand Syndrome: The “Hemostatic” Waring Blender Syndrome. JAMA Cardiol. 2016;1(2):205–206. doi:10.1001/jamacardio.2016.0182
Goltstein LCMJ, Rooijakkers MJP, Görtjes NCC, Akkermans RP, Zegers ES, Pisters R, van Wely MH, van der Wulp K, Drenth JPH, van Geenen EJM, van Royen N. Reduction of Gastrointestinal Bleeding in Patients With Heyde Syndrome Undergoing Transcatheter Aortic Valve Implantation. Circ Cardiovasc Interv. 2022 Jul;15(7):e011848. doi: 10.1161/CIRCINTERVENTIONS.122.011848. Epub 2022 Jul 5. PMID: 35861798; PMCID: PMC9287099.
Aortic valve stenosis, a precipitating factor of recurrent bleed in colonic angiodysplasia: a literature review. Johnson AM, Chovwen PE, Akpan EJ, Patel A. Cureus. 2021;13
Jamil D, Tran HH, Mansoor M, Bbutt SR, Satnarine T, Ratna P, Sarker A, Ramesh AS, Munoz Tello C, Mohammed L. Multimodal Treatment and Diagnostic Modalities in the Setting of Heyde's Syndrome: A Systematic Review. Cureus. 2022 Aug 16;14(8):e28080. doi: 10.7759/cureus.28080. PMID: 36127959; PMCID: PMC9477546.
Review article: gastrointestinal angiodysplasia - pathogenesis, diagnosis and management. Sami SS, Al-Araji SA, Ragunath K. Aliment Pharmacol Ther. 2014;39:15–34.
Hudzik B, Wilczek K, Gasior M. Heyde syndrome: gastrointestinal bleeding and aortic stenosis. CMAJ. 2016 Feb 2;188(2):135-138. doi: 10.1503/cmaj.150194. Epub 2015 Jun 29. PMID: 26124230; PMCID: PMC4732965.
Loscalzo J. From clinical observation to mechanism--Heyde's syndrome. N Engl J Med. 2012 Nov 15;367(20):1954-6. doi: 10.1056/NEJMcibr1205363. PMID: 23150964.
Ng C, Motto DG, Di Paola J. Diagnostic approach to von Willebrand disease. Blood. 2015 Mar 26;125(13):2029-37. doi: 10.1182/blood-2014-08-528398. Epub 2015 Feb 23. PMID: 25712990; PMCID: PMC4375103.
Rana M. Aortic Valve Stenosis: Diagnostic Approaches and Recommendations of the 2021 ESC/EACTS Guidelines for the Management of Valvular Heart Disease -A Review of the Literature. Cardiol Cardiovasc Med. 2022 Jun;6(3):315-324. doi: 10.26502/fccm.92920267. Epub 2022 Jun 27. PMID: 36035621; PMCID: PMC9410571.
UK TAVI Trial Investigators; Toff WD, Hildick-Smith D, Kovac J, Mullen MJ, Wendler O, Mansouri A, Rombach I, Abrams KR, Conroy SP, Flather MD, Gray AM, MacCarthy P, Monaghan MJ, Prendergast B, Ray S, Young CP, Crossman DC, Cleland JGF, de Belder MA, Ludman PF, Jones S, Densem CG, Tsui S, Kuduvalli M, Mills JD, Banning AP, Sayeed R, Hasan R, Fraser DGW, Trivedi U, Davies SW, Duncan A, Curzen N, Ohri SK, Malkin CJ, Kaul P, Muir DF, Owens WA, Uren NG, Pessotto R, Kennon S, Awad WI, Khogali SS, Matuszewski M, Edwards RJ, Ramesh BC, Dalby M, Raja SG, Mariscalco G, Lloyd C, Cox ID, Redwood SR, Gunning MG, Ridley PD. Effect of Transcatheter Aortic Valve Implantation vs Surgical Aortic Valve Replacement on All-Cause Mortality in Patients With Aortic Stenosis: A Randomized Clinical Trial. JAMA. 2022 May 17;327(19):1875-1887. doi: 10.1001/jama.2022.5776. PMID: 35579641; PMCID: PMC9115619.