Case Presentation:
During your shift in the CCU, you admit a 47 year old male with PMH of HFrEF (EF 40%) secondary ICM with recent stent to the RCA in the setting of a STEMI (~5 months ago), paroxysmal afib on apixaban, HTN, CKD stage 3, PVD, and T2MD who presents with SOB, new DOE, and weight gain thought to be in acute decompensated heart failure. You are putting in the patient’s admission orders when you realize he has been taking apixaban, clopidogrel, and aspirin for the past 5 months.
Ask Yourself:
Questions:
1. Which of these medications would you continue? Which would you stop?
2. For the medications that you are continuing, how long will you continue them for?
3. What other considerations need to be made prior to discontinuing these medications?
Background:
Two main categories of medication in cardiology are the antiplatelets and the anticoagulants (AC). Whether we are trying to prevent thrombosis from afib or stent stenosis with plavix, these two groups of drugs are now commonly prescribed as they have been shown time and time again to be effective. Unfortunately, these medications are not without side effects (namely bleeding), and thus require careful consideration regarding choice of particular medication and the length of therapy needed. Many of our patients often have multiple indications to be on both antiplatelet and anticoagulation, so understanding how to balance the two and when to stop prescribing one is imperative.
The picture above shows how stable coronary artery disease (CAD) progresses to full occlusion due to acute plaque rupture. When there is endothelial damage, the body tries to maintain hemostasis by both primary hemostasis and secondary hemostasis. Platelets will aggregate to form a platelet plug (via primary hemostasis). The platelet plug then gets stabilized by the fibrin mesh from the coagulation cascade (from secondary hemostasis).
Refresher:
There are two arms in the antithrombotic therapy:
1. Anticoagulation: Meant for lower velocity disease states (i.e. afib stroke prophylaxis, pulmonary embolism, DVT)
A DOAC (direct oral anticoagulant) / NOAC (Non-Vitamin K Oral Antagonists Oral Anticoagulants) are medications that either directly inhibit thrombin (i.e. Dabigatran) or Factor Xa (rixaroxaban, apixaban, edoxaban) as seen in the figure to the left.
Vitamin K antagonist (aka warfarin): Used mainly for mechanical heart valves, rheumatic mitral stenosis, valvular atrial fibrillation, and when patients fail a NOAC/DOAC (i.e. they still have a DVT or thromboembolism despite religiously taking their AC).
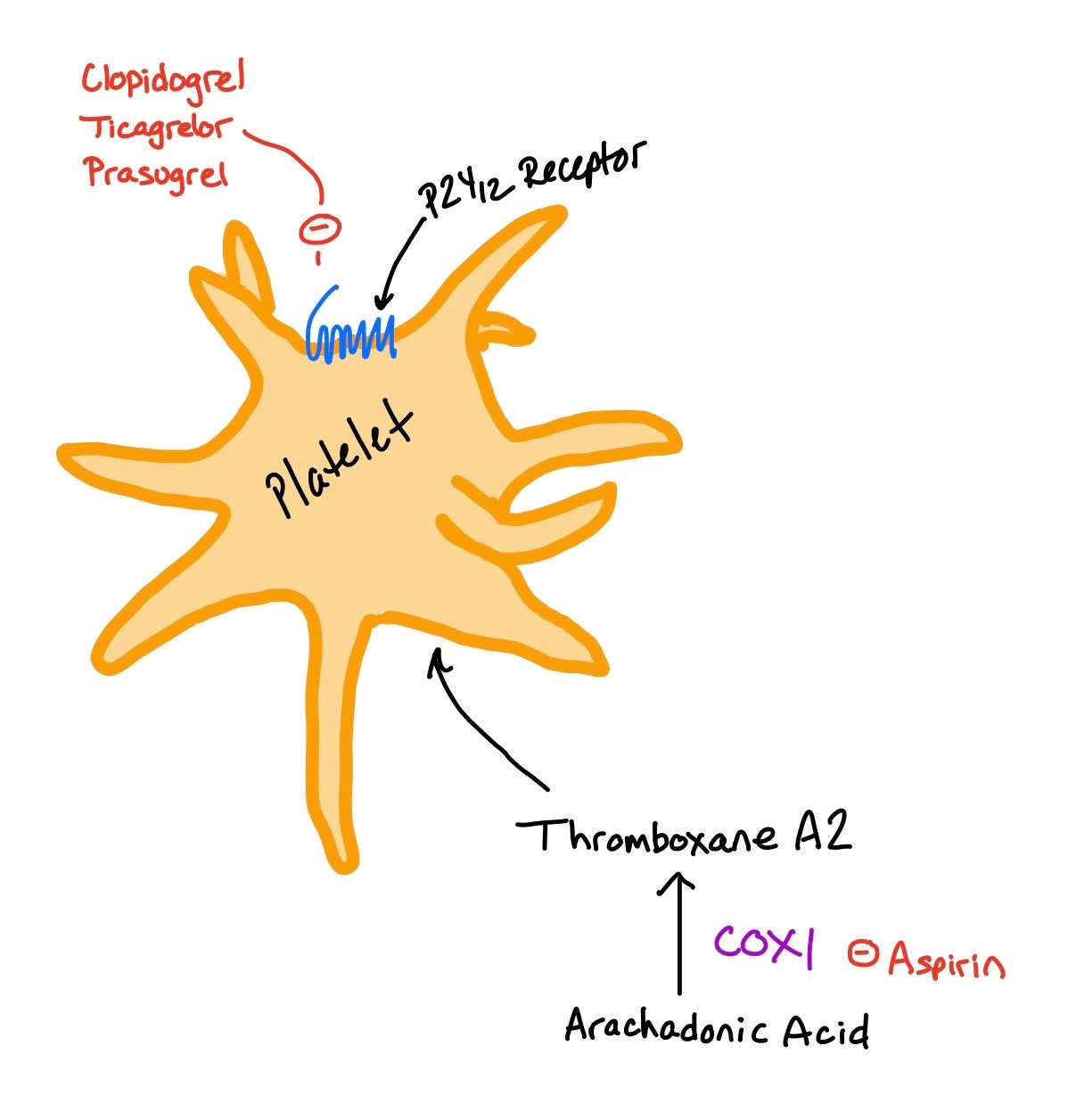
2. Antiplatelet (aka P2Y12 inhibitors / COX1 inhibitors): Used more in higher velocity disease states like CAD, PAD, and CVA. Examples include aspirin (ASA), clopidogrel, prasugrel, ticagrelor.
Common P2Y12 Inhibitors:
Clopidogrel (Plavix)
Ticagrelor (Brillenta)
Prasugrel (Effient)
** REMEMBER! While in a similar class, these medications are not equal! If changing between different P2Y12 inhibitors, the patient must be reloaded! See AHA figure
COX1 Inhibitor (aka Aspirin)
This figure shows how the P2Y12 inhibitors (i.e. Clopidogrel, Ticagrelor, Prasugrel) bind to the P2Y12 receptor to prevent platelet activation. Similarly, Aspirin inhibits COX 1 and 2, ultimately preventing additional platelet activation..
The figure above is from the AHA shows how to transition from the different P2Y12 inhibitors on the agents and the timing from the stent.
Dual Anti-platelet Therapy (DAPT):
In most situations, dual therapy (i.e. AC + antiplatelet) is enough. However, when a patient is considered high risk (i.e. high burden of vascular disease, multiple stent placement, history of multiple MIs, etc), the decision may be made to continue the patient on triple therapy.
When comparing dual therapy to Triple therapy (i.e. DAPT + anticoagulation), there was no reduction in ischemic outcomes. However, triple therapy has been shown to have increased bleeding risk. As such, it should only be used in patients with very high ischemic risks and only for a short period of time (4-6 weeks max). If the decision is made to start the patient on triple therapy, they should get Aspirin 81mg, a P2Y12, and an additional non-warfarin anticoagulant. Anything beyond the 4-6 weeks of triple therapy is NOT evidence based or recommended.
Remember, any of these patients on 2 or more thrombotic agents should get a PPI in order to help reduce bleeding events! They should also avoid NSAIDs for the same reason.
OK to hold DOAC 36-48 hours prior to PCI
Any patient who has had an ACS, whether they got a stent or not, should should receive up to 12 months of DAPT as they are thought to be prothrombotic. In contrast, patients who got a stent in a non-ACS setting can have their DAPT stopped after 6 months. In specific scenarios of patients having very high bleeding risks based on individual risk assessment, duration of DAPT may be adjusted. In some cases, patients may only be on DAPT for 1-3 months.
The associated picture does a great job differentiating indications of anti-platelets vs anticoagulants. Determining whether the medication is needed for a high velocity vs low velocity state helps helps determine which medication to use.
1. Approximately 10% of patients with recent PCI have concomitant AF. Others may have concomitant VTE. Choosing the optimal antithrombotic regimen can be a challenge.
2. Clinical pathways are suggested for four potential clinical situations: (1) prior AF on anticoagulation and the need for PCI; (2) new-onset AF requiring anticoagulation in a patient already on antiplatelet therapy for coronary artery disease (CAD); (3) prior VTE on anticoagulation and the need for PCI; and (4) new or recurrent VTE requiring anticoagulation in a patient already on antiplatelet therapy for CAD.
3. In general, the use of “triple therapy” (dual antiplatelet therapy plus anticoagulation) is not recommended for most patients due to an increased risk of bleeding. If triple therapy is needed, a short duration (e.g., no more than 30 days) is recommended. When combined with an anticoagulant, clopidogrel is the recommended antiplatelet agent for most patients. If aspirin is being used, it should be limited to <100 mg daily dosing.
4. For patients taking ≥2 antithrombotic agents, starting or continuing a proton pump inhibitor and avoiding other anti-inflammatory medications should be employed to reduce gastrointestinal bleeding risk.
5. For patients with AF on anticoagulation who need a PCI, use of a direct oral anticoagulant (DOAC) is preferred over a vitamin K antagonist (VKA) when appropriate. Oral anticoagulation plus P2Y12 antiplatelet combination is recommended for the first 6-12 months (potentially switching P2Y12 to aspirin for months 6-12 if PCI for stable ischemic heart disease), followed by anticoagulation monotherapy after 12 months.
6. For patients on antiplatelet therapy who develop new AF, management depends on the indication for antiplatelet therapy. For primary cardiovascular prevention, switch to anticoagulation monotherapy is recommended. For PCI with stable ischemic heart disease or acute coronary syndrome, use of oral anticoagulant plus a P2Y12 inhibitor for no more than 12 months is recommended, followed by oral anticoagulation alone. For patients with cerebrovascular disease without carotid stenting, oral anticoagulation monotherapy is recommended. For patients with carotid stenting or peripheral artery disease, a short course of anticoagulation plus P2Y12 inhibitor may be recommended, followed by oral anticoagulation alone.
7. Management of patients with prior VTE depends on the clinical situation during which the VTE event occurred. If the VTE was associated with strongly provoking, reversible risk factors, then delaying a PCI may be beneficial so that anticoagulation therapy can be discontinued. If long-term/indefinite anticoagulation is required, then use of standard treatment doses of anticoagulation plus P2Y12 inhibitor antiplatelet therapy are recommended following PCI. If the dose of anticoagulation is reduced (e.g., “half-dose DOAC” for VTE secondary prevention), then continued use of a single antiplatelet medication (e.g., aspirin) is indicated long-term.
8. For patients on antiplatelet therapy who develop a new VTE event, use of anticoagulation plus single antiplatelet medication is generally recommended. Patients using antiplatelet therapy for primary cardiovascular disease prevention or >12 months from the most recent PCI or acute coronary syndrome can be treated with anticoagulation monotherapy.
9. For patients taking DOAC medications who require PCI, most DOACs can be held for no more than 36-48 hours prior to the procedure. Holding a DOAC for longer periods of time may be required for patients with moderate-severe renal dysfunction, especially if using dabigatran.
10. When used in combination with antiplatelet medications, dosing of DOAC medications usually follows the Food and Drug Administration guidance for stroke prevention in AF or treatment of VTE. However, rivaroxaban may be administered at 15 mg daily (reduce to 10 mg daily for creatinine clearance <50 ml/min) when combined with P2Y12 inhibitors, based on the PIONEER-AF PCI study.
2025 ACS Updates
P2Y12 Inhibitors: When thinking about P2Y12 inhibitors, there are three main medications: ticagrelor, prasugrel, and clopidogrel. When patients present with ACS, the guidelines recommend ticagrelor or prasugrel as they had decreased major adverse cardiac events (MACE) and stent thrombosis as compared with clopidogrel.
The figure above from the updated 2025 ACS Guidelines shows which P2Y12 Inhibitor is preferred when patients come in with ACS, CABG, have not had any invasive intervention, or were initially treated with fibrinolytic therapy.
When thinking about length of anti-platelet therapy, the guidelines have changed in regards to patients who are at higher bleeding risk. Generally speaking, the guidelines prefer 12 of months DAPT therapy when patients present with ACS. If they are very high bleeding risks, PPI should be used. Additionally, they can potentially continue DAPT therapy for 1 month post-PCI and continue ticagrelor monotherapy after 1 month. See the chart below for more details.
Back To The Case:
1. Which of these medications would you continue? Which would you stop?
This patient is currently on triple therapy, which should never be continued for more than 4-6 weeks as it has very high bleeding rates. Continue the patient’s apixaban for his afib, but STOP one of the aspirin.
2. For the medications that you are continuing, how long will you continue them for?
Once the patient has been on the clopidogrel and apixaban for 12 months, you can STOP the clopidogrel and continue with the apixaban indefinitely. Note! If this patient got a stent that was NOT in the setting of ACS, you could stop the clopidogrel earlier after 6 months.
3. What other considerations need to be made when discussing the patient’s medications?
Make sure the patient is on a PPI if they are on both an antiplatelet and AC! Also, make sure to document stop dates for the medications! If you don’t do it, the patient may be on this medication indefinitely as people tend to not feel comfortable stopping antithrombotics started by cardiology!
If this patient develops worsening of his PVD, you can always add the antiplatelet back on with the apixaban!
Further Learning:
Resident Responsibilities
→ Before restarting any antithrombotic therapy, make sure you know then indications. Many times, people tend to just continue medications that other physicians started, like aspirin or plavix.
→ If you are part of the team starting any antiplatelet or anticoagulant, make sure to write and end date for when you want the patient to STOP taking this medication. This will make it easier for future providers to ensure the patient is on the correct medication.
→ If a patient has a high risk of GI bleeding, according to the ACCF/ACG/AHA guidelines, they should be treated with a concurrent PPI. If bleeding risks are low, there are no definitive guidelines for PPI.
→ Prior to picking a P2Y12 inhibitor, consider cost differences between the medications. Remember! If patients cannot afford their medications and will therefore not take them, it isn't a good medication for them.
Attending / PharmD Pearls
- In the peri-PCI period, patients may be on triple therapy (i.e. DAPT+AC) during their hospital stay for ~1 week as this is the highest ischemic risk time period. However, prior to discharge, STOP the aspirin so patients are only leaving on a P2Y12 inhibitor and AC!!
-When patients need a P2Y12 inhibitor in addition to oral anticoagulation (i.e. apixaban), clopidogrel is the agent of choice
-Make sure to include when and where the stent was placed in your assessment, as well as stop dates for DAPT.
-Note that stents placed with STEMIs vs planned PCIs have different DAPT therapy lengths (12months vs 6 months).
- Clopidogrel and Prasugrel is a thienopyridine, which means it has a sulfer group in it. Therefore, if someone has a sulfer allergy, try Ticagrelor or Cangrelor would be better options.
-Clopidogrel is a pro-drug that requires the CYP 2C19 enzyme activity in order for the drug to work. Therefore, we test this enzyme activity to ensure the drug will work!
Further Reading
PIONEER-AF PCI Study–Rivaroxaban 15mg qdaily + P2Y12 inhibitor vs vitamin K antagonist + DAPT showed lower incidence of bleeding in the patients on Rivaroxaban with no significant increase in ischemic events or thrombosis.
ISAR-REACT 5- Patients with ACS who required stenting did slightly better with prasugrel vs ticagrelor with 2.4% absolute reduction in death, nonfatal MI, and stroke. Major bleeding rates were similar.
AUGUSTUS Trial–Compares the efficacy of anticoagulants and antiplatelet regimen in patients with afib who underwent PCI or ACS. Overall, pts on a P2Y12 inhibitor + apixaban had fewer major bleeding events without significant difference in ischemic events than those on oral vitamin K antagonists and / or aspirin.
ENTRUST-AF PCI Trial- Edoxaban / clopidogrel was noninferior to vitamin K agonist triple therapy.
COMPASS Trial– In patients who have significant atherosclerotic disease (i.e. PVD, CAD, etc), using low dose anticoagulation (like rivaroxaban) + aspirin was shown to have decreased ischemic events and cardiovascular mortality.
TRITON-TIMI 38, PLATO, and ISAR-REACT 5- Three landmark trials differentiating clopidogrel vs prasugrel vs Ticagrelor
WOEST Trial found that patients on anticoagulation undergoing PCI had significantly less bleeding when only clopidogrel was added vs clopidogrel + aspirin.
RE-DUAL PCI– In patients who got a stent who had nonvalvular atrial fibrillation, dabigatran + a P2Y12 inhibitor had fewer bleeding events when compared with triple therapy of warfarin, P2Y12 inhibitor, and ASA. When looking at thromboembolic risks, dabigatran + a P2Y12 inhibitor was noninferior to triple therapy
How’d we do?
The following individuals contributed to this topic: Rebecca Garber, MD, Stephanie Dwyer, PharmD, Jinjoo Chung, PharmD
Chapter Resources
https://www.nejm.org/doi/full/10.1056/NEJMoa1817083
Augustus trial
2020 Expert Consensus guided to AC and antiplatelets
https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.117.031164
How to switch between P2Y12 inhibitors!
https://jamanetwork.com/journals/jama/article-abstract/2736563
DAPT for 1 month followed up plavix vs DAPT for 12 months followed by ASA
https://www.coreimpodcast.com/2021/04/07/5-pearls-on-dual-antiplatelet-therapy/
Further listening
Image
Image
NOAC vs Warfarin picture
Need for PPI when on DAPT
https://www.ahajournals.org/doi/full/10.1161/circulationaha.117.031164
How to transition between different P2Y12 inhibtiors